It is interesting to me (and likely only me) that depending on the words or phrases used in a conversation, something can be construed as good or bad — even if both statements are saying the same thing. Why might I say this?
When a cat owner hears that their cat has the medical condition hepatic lipidosis, it doesn’t sound too bad, especially when one may not know the meaning of both words.
The words have almost a pleasant rhythm to them. BUT, if you are told your cat has fatty liver disease, it sounds considerably worse because ‘fatty’ and ‘disease’ have such negative connotations associated with them.
Regardless of which terminology is used, hepatic lipidosis or fatty liver disease, it is a serious and debilitating condition in cats that can be fatal.
It is critical for anyone who has a cat to know about this condition, understand how it happens, and the steps to take to treat and prevent it.
Read on to learn more about this common liver disease that is unique to cats.
Skip to section:
What Is Fatty Liver Disease (Hepatic Lipidosis) in Cats?
The liver performs many essential functions to sustain your cat’s life. Without a properly functioning liver, it is not possible to live.
What a Cat’s Liver Does
• Makes proteins required to help the blood clot normally• Makes proteins required to help maintain fluid balance and blood pressure within the body
• Makes bile, which is essential for overall fat metabolism within the body, as well as for removing certain metabolic byproducts and toxins from the body
• Detoxifies blood coming from the digestive tract
• Stores essential vitamins and minerals
• Converts ammonia (a toxic byproduct of protein metabolism) into urea — a less harmful compound, which is more easily cleared from the body by the kidneys
The liver is divided into sections (lobes). Each section is made up of lobules, which are tiny structural and functional units. The cells that make up the lobules are called liver cells (hepatocytes).
Hepatic lipidosis occurs when there is an accumulation of triglycerides (the most common form of fat in the blood) in the liver cells. When this happens, the liver can’t function as it needs to.
What Causes the Fat to Accumulate?
While a cat can get 'primary hepatic lipidosis' (the disease with no cause), in 90% of the cases, it is caused by some other underlying condition. See those conditions and diseases listed below.
It is pretty likely that many of the 'primary' cases actually have an underlying cause, but it's just not detected or diagnosed.
The reason for hepatic lipidosis being a secondary condition is most of the primary or underlying conditions cause anorexia (loss of appetite).
When cats stop eating for 3 to 4 days, excessive fat that is stored throughout the body is broken down more quickly in order to provide the cat with energy and nutrients. Their liver becomes overloaded, and it can’t process the fat properly.
This results in the buildup of fat within and around the liver cells. The result is an obstruction of the liver's functions.

Common Conditions That Cause or Increase a Cat's Risk of Hepatic Lipidosis
- Obesity
- Diabetes
- Hyperthyroidism
- Inflammatory bowel disease
- Respiratory disease
- Liver disease
- Kidney disease
- Pancreatitis
- Cancer
- Pain
- Anxiety
While the condition can affect cats of all ages and weights, the incidence appears to be considerably higher in overweight and obese cats as well as middle-aged cats.
Signs of Liver Dysfunction or Failure in Cats
Because the liver is involved in so many body functions, the symptoms you might see when your cat suffers from hepatic lipidosis or any other condition that causes liver dysfunction can vary widely. Below are some of the signs that could indicate a problem with your cat's liver.
- Yellowing of the ears, eyes (whites), gums, or skin (jaundice)
- Decreased energy
- Decreased appetite
- Note: Affected cats will avoid their food bowls completely and even appear scared of them.
- Increased thirst
- Increased urination
- Increased salivation
- Vomiting
- Small, pin-sized bruises on gums, ears, or elsewhere on the body (petechiae)
- Large bruises under the skin
- Nose bleeds
- Blood in urine or stool
- Breathing difficulties
- Swollen abdomen
- Seizures

Questions? To chat with a veterinarian about your cat and fatty liver disease, Click here
How Fatty Liver Disease Is Diagnosed in Cats
If your veterinarian suspects your cat has fatty liver disease after obtaining a detailed medical history and performing a physical examination, they will recommend blood tests and possibly an ultrasound and liver biopsy.
The blood tests are used to determine liver function as well as to diagnose any other underlying medical issues.
The ultrasound is essential in determining if there is liver enlargement and to evaluate any other potential causes.
The liver biopsy is used to determine if there is an increased amount of fat around and within the liver cells. Liver biopsies can be obtained in a few ways. While your cat is under sedation, an ultrasound is used to guide the needle into your cat’s liver in order to obtain a sample of the liver and its cells.
A liver biopsy can also be obtained laparoscopically. This requires a cat to be completely anesthetized. Lastly, if an exploratory surgery is needed and the liver appears abnormal, the surgeon can take an adequate section of liver for biopsy.
Treatment for Fatty Liver Disease
If not treated promptly and aggressively, this condition can be fatal. Therefore, if your cat refuses to eat for more than 2 days and/or has any of the symptoms listed above, seek veterinary care immediately.
Cats are generally hospitalized in order to receive aggressive nutritional support and intravenous fluids to correct electrolyte imbalances and dehydration.
Nutrition support can involve intravenous nutrients, administration of vitamins, and possibly a feeding tube. This high level of nutritional support is done until the cat’s normal appetite returns and the liver resumes its normal function and can release the excessive fat stores. This typically takes about 6 to 7 weeks.
Additional treatments can include medications to aid liver function, as well as control nausea, vomiting, and pain.
All underlying medical conditions that caused the hepatic lipidosis need to be treated and managed as well in order for a full recovery to be possible.
Your cat may be hospitalized the entire time, or a feeding tube may be placed so nutritional support and care can be managed at home.
How to Prevent Hepatic Lipidosis in Your Cat
Since some of the underlying causes are preventable or, at least, treatable in most cases of hepatic lipidosis in cats, it means that there are several things you can do to protect your cat and minimize their chances of suffering from a bout of this disease.
These are the steps to take.
Maintain a Healthy Body Weight for Your Cat
Since overweight and obese cats have more fat 'stores' within their body to mobilize and deposit in their liver, excessive weight can be one of the most significant risk factors for your cat to develop fatty liver disease.
If your cat has a little extra 'fluff in their coat,' you’re not alone. Pets in the United States are overweight and continuing to get more overweight.
The Association for Pet Obesity Prevention found that 61% of cats in the U.S. are overweight or obese. This is probably because many cat owners like to spoil their cats, indoor cats don’t often get much exercise, and not everyone knows what their cat’s weight should be or how much to feed their cat. Here are some simple steps you can take to get your indoor cat moving.
In between vet visits (when your vet will usually tell you if your cat is overweight or underweight), you can 'feel out' whether your cat is the ideal body weight. Use this body condition chart to assess your cat's weight.
How to Tell if Your Cat is Overweight
- Your cat should have a discernible waist that, when viewed from the side, tucks up toward the back of the legs.
- You should be able to feel your cat’s ribs easily without having to press through a thick layer of fat.
- Your cat’s back should not be perfectly flat.
- Your cat should not have 'love handles.
Learn more about identifying and preventing obesity by reading our article, Helping Your Overweight or Obese Cat.
Questions? To chat with a veterinarian about your cat and fatty liver disease, Click here

Keep an Eye on How Well Your Cat is Eating
To prevent fatty liver disease, you need to make sure your cat isn’t too fat but also that they’re eating an appropriate amount.
A decreased or sudden halt in eating is almost always seen in cats with this disease. You shouldn’t think that you can 'out stubborn' your cat by waiting for them to get hungry and start eating again. They will always win this game, which actually means that you’ll both lose.
For this reason, you should keep an eye out and always make sure your cat is eating an appropriate amount for their body type and size. If your cat needs to go on a diet, do so gradually and consult with your vet before making any dietary changes.
If your cat suddenly seems less interested in their food…
- Talk to your vet early, as a lack of appetite is rarely a good sign
- Take steps to tempt their appetite
You can find excellent tips in our article, Your Cat Won’t Eat! Tips and Reasons Why.
Introduce Diet Changes Gradually to Your Cat
Drastic or sudden changes to diet can upset your cat’s digestive system or even cause them to lose interest in eating, both of which can then lead to fatty liver disease.
If you need to transition your cat to a new food, do so slowly (in some cases, very slowly) and start them on a mixture of the new and old food.
Over the course of 1–2 weeks, gradually blend in more of the new food with the old food so your cat can adjust (both their taste buds and their gut). With a little patience, you can make the transition without turning your cat off their new food.
Some cats can make the transition over a week, while others might require a little more time to switch foods (hence the longer timeframes in the parenthesis below).
How to properly change your cat’s food
- Days 1–2 (or days 1–4): Mix 25% new food with 75% old food
- Days 3–5 (or days 5–10): Mix 50% new food with 50% old food
- Days 6–7 (or days 11–14): Mix 75% new food with 25% old food
Don’t Leave Your Cat Home Alone
Though cats generally have reputations as 'loners' and 'low maintenance' pets, cats are typically neither. Most cats really do like to be around people. Oftentimes, even more than they like to eat food, play with toys, or have catnip!
If your cat is one of the social ones — and the odds are good that they are — even leaving them alone without any human interaction or supervision for a 'quick weekend' away can cause them stress and lead to problems like decreased food access and eating, urinary obstruction, and a host of others.
Even if you’re only leaving for a couple of nights, getting a pet sitter or at least someone who will reliably stop by once to twice a day to scoop litter boxes, check-in, feed, and play with your cat is important.
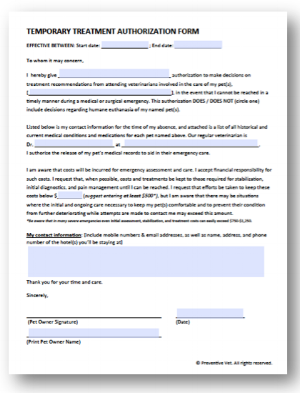
Download this pet sitter treatment authorization form. If something happens to your cat while away, your sitter can get them the veterinary care they need.
Stay on Top of Your Cat’s Health and Conditions
Early detection of any underlying condition allows for prompt treatment and management. This improves your cat’s well-being sooner and decreases the chances they will suffer from hepatic lipidosis.
Since some of the underlying conditions are more likely in older or senior cats, being sure to have them evaluated by their veterinarian at least yearly (ideally every six months) is critical. Remember, things can change quickly, especially as cats get older.

Limit Your Cat’s Stress
Stress and anxiety can be a big contributing factor to fatty liver disease in cats, as stressed and anxious cats often don't eat well. And, just like with people, stress can worsen existing health issues. So, it’s always a good idea to take steps to help your cat manage stress.
Some of the most common sources of kitty stress include:
- Sudden changes to their environment
- Not getting along well with other pets or people in the home
- Adding a new baby, adult, or pet to the home
- Feeling pain or discomfort from medical issues
- Exposure to specific fear triggers like loud sounds (fireworks) or strangers (holiday guests)
How can you tell if your cat is stressed? If you’ve got a generally anxious cat who has always been skittish, reactive to movement and sounds, and hesitant to move freely through the home, stress and fear are probably key factors.
On the other hand, if your cat is usually easy-going and confident, you’ll notice changes in their normal behavior when stress becomes an issue. They may become less affectionate, more nervous, on alert during meals, less playful, etc.
Not only can these changes be a sign of stress, but they can also be indicative of pain or discomfort from medical issues.
Once you know there are no medical issues (or they are managed) that are causing your cat stress, consider consulting with a veterinary behaviorist or a certified feline training and behavior consultant. They will help you determine what may be causing stress for your cat and develop a plan to help them feel better about those triggers and generally build their confidence.
If you know what’s stressing your cat out, remove those triggers if possible. And encourage stress reduction naturally through play, mental enrichment, and affection.